|
Are we hyping infection control inside clinics?

By Shobha Shukla, CNS
July 23, 2014
The author is the Managing Editor of Citizen News Service - CNS. She is reporting from the XX International AIDS Conference (AIDS 2014) with support from the World Health Organization (WHO) Global Tuberculosis Programme. She is a J2J Fellow of National Press Foundation (NPF) USA and received her editing training in Singapore. She has earlier worked with State Planning Institute, UP and taught physics at India's prestigious Loreto Convent. She also co-authored and edited publications on gender justice, childhood TB, childhood pneumonia, Hepatitis C Virus and HIV, and MDR-TB. Email: shobha@citizen-news.org, website: www.citizen-news.org
Tuberculosis (TB) is an infectious bacterial disease and spreads through the air. When people with pulmonary TB cough, sneeze or spit, they propel the TB germs into the air and a person needs to inhale only a few of these germs to become infected. On the other hand, HIV/AIDS is a viral disease that is transmitted chiefly through unprotected sexual intercourse and contaminated blood. Yet there is a deadly synergy between the two, with people living with HIV (PLHIV) being 30 times more likely to develop TB and one in every five deaths in them being attributable to TB.
Thus integrating TB-HIV services is imperative to stemming the tide of both these diseases. During a high level WHO consultation held in conjunction with the XX International AIDS Conference (AIDS 2014) in Melbourne (that analysed the barriers in integrating TB and HIV programmes for the elimination of TB-HIV deaths), the preferred ‘one stop model’ for dispensing both TB-HIV services raised an interesting discussion about infection control methods to prevent the spread of the airborne TB infection within healthcare facilities providing HIV services.
While participants from Cambodia, Vietnam and India stressed upon the importance of infection control methods within clinical settings, a thought provoking comment from Prof Linda-Gail Bekker, of the Desmond Tutu HIV Centre, University of Cape Town, raised the issue about whether we were creating an undue hype about infection control inside hospital/clinical settings when patients are actually spending more time outside these facilities in their homes, in churches, in buses and in other public places—sharing the same air. She wondered that, “Is there any evidence that we are placing our patients at risk of TB in hospital/clinic settings so that we devote a whole lot of time to infrastructural requirements to control infection within these premises? The risk which patients have of catching infection while coming to the HIV clinic in closed taxis and vehicles could be much greater than sitting for a few minutes in a clinic.”
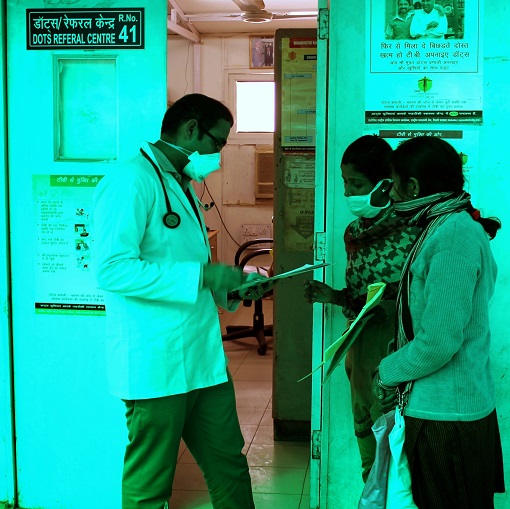
Dr BB Rewari from Department of AIDS Control, Ministry of Health and Family Welfare, Government of India, insisted that, in a country like India, PLHIV do spend a lot of time (1-3 hours) at overburdened HIV centres providing antiretroviral therapy (ART) facilities. So the chances of their getting TB infection are very much present there. Dr Rewari informed that, “Infection control depends upon structural issues that are difficult to tackle, but some of the measures taken in India at ART centres are –teaching about cough etiquette; giving priority to coughing PLHIV patients in drug dispensing and symptom screening; providing face masks at the entrance of each ART centre; decentralisation of services to reduce patients’ visit to the main centres; providing IPT services (which will be soon rolled out in India) at TB sites (just as it is being done for cotrimoxazole prophylaxis therapy - CPT) to prevent overcrowding at ART centres. All this will help in reducing airborne infection at tertiary care facilities and district hospitals.”
Dr Mean Chhi Vun from National Center for HIV/AIDS, Dermatology and STD, Cambodia, felt that infection control should be integrated in the general health care system and not just in TB and/or HIV services.
Dr Nguyen Hoang Long of Vietnam Administration of HIV/AIDS Control, Vietnam, said it was important to educate TB and other patients on infection control.
Dr Haileyesus Getahun, Coordinator (TB-HIV and community engagement), WHO Global Tuberculosis Programme, in an interview given to Citizen News Service (CNS), agreed that simple healthcare and infection control measures followed at the community and individual level can go a long way in stemming the spread of airborne TB infection. He said that, “There is evidence for PLHIV getting their TB infection outside of health facilities. People are spending more time in contact with others in non-clinical settings. In some African countries there are public TB campaigns for commuters to keep the windows open while travelling. This has been a big (and positive) behavioural change.”
He however added that, “We cannot ignore infection control practices in clinical settings. Infection control is a sound clinical practice and must be integrated into routine clinical behaviour and practiced by all clinicians. In some resource limited settings clinicians, at times, sit in dingy, dark and small rooms with poor ventilation. We have to take all administrative measures like putting cough monitors, and identifying those who are coughing as soon as they come to the clinical setting. At times it is also a question of behaviour and attitude on part of the clinicians.”
We must remember that a lot many PLHIV are catching TB from those who are HIV negative and so infection control measures at community and household level should be given as much (if not more) importance as within healthcare settings. The time spent and the risk involved in sharing the air with others at home with HIV negative but TB infected family members, or inside jam packed transport facility or in other public places cannot be written off.
It is true that in many settings TB and HIV services are not being brought together because of the fear of exposing the TB non infected PLHIV to TB infection due to lack of proper infection control measures in place. At the same time, one needs to seriously discuss whether we are neglecting infection control in families and public places and hyping it for hospitals alone.
There is definitely a need to have better health and hygiene education and awareness in the masses and also in healthcare staff about simple infection control measures. Curbing coughing and spitting in public places --a very common practice in India—and having properly ventilated homes and transport facilities will definitely complement infection control measures inside health clinics in controlling air borne infections like TB.
--- Shared under Creative Commons (CC) Attribution License
Posted on: July 23, 2014 09:22 AM IST
|